Malignant tumors are complex biological systems that depend on their ability to restructure their microenvironment. A key role in this process is played by macrophages, innate immunity cells that normally detect and destroy pathogens and help T-lymphocytes have a cytotoxic effect on tumors. However, inside tumor tissue, macrophages more often take on the M2 phenotype, which has regenerative properties and suppresses cytotoxic T-lymphocytes, thus promoting tumor growth. The antivirus and anticancer M1 macrophages are almost absent in tumor tissue.
Unlike the majority of targeted methods that aim to destroy cancer cells directly, the new system targets a tumor’s immune environment. Instead of a direct attack on a tumor, the researchers suggest “reprogramming” the immune cells that support it by switching macrophages from the M2 to M1 phenotype and activating the body’s own anti-tumor immunity.
The key feature of the new technology is the distant activation of an immunomodulating substance with near-infrared laser radiation, which significantly decreases the risk of side effects and undesirable immune system activation outside the tumor. The solution is a single complex, where each element performs a clearly defined function:
- Polymer carriers act as medication containers. They were created in two sizes (micrometer and submicrometer) in order to study how size affects the cell capture and immune response efficiency;
- Gold nanorods built into the carrier shells act as transformers of the external stimulus. They absorb infrared radiation, thus causing localized overheating in capsule shells and releasing the treatment;
- The active substance (STING agonist) is a powerful immunomodulator that activates innate antitumor immunity.
In a way, the new method is akin to remotely controlled pinpoint surgery. Once the capsules are introduced into the tumor, they are subjected to a laser; the nanorods absorb the infrared light, heat up, and locally damage the polymer shells; as a result, the treatment is released at precisely the necessary time and place. Once released in a tumor’s microenvironment, the immunomodulator launches a chain of biochemical reactions that “switch” macrophages from the M1 to the M2 phenotype. Without laser activation, the capsules remain stable, inactive, and safe.
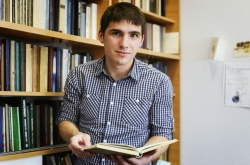
“In this study, we demonstrate that we can remotely control treatment release and the moment of its activation. After injection, the drug will remain inactive until we point a laser at the necessary location. This is the main advantage of using a laser in this method: thanks to such precise control, we can minimize side effects and prevent undesirable impact on healthy tissue,” shares Lidia Mikhailova, a junior researcher at ITMO’s Faculty of Physics and the key author of the paper.

Schematic of macrophage reprogramming when subjected to laser radiation. Image courtesy of the researchers
During lab testing on a macrophages culture (in vitro), 85-88% of cells switched to the M1 phenotype after laser activation. During in vivo experiments on melanoma models in mice, the share of switched M1 cells reached 28.3%. This difference in results occurs because a living organism is more complex, with barrier tissues, immune reactions, and metabolic processes that hinder particle delivery and lower their concentration. However, the in vivo data offer a more accurate look at the method’s potential clinical applicability. At the same time, the larger, micrometer-size capsules turned out to be more effective compared to the submicrometer ones, which has to do with their bigger capacity and more selective capture of tumor macrophages.
“This project unites the expertise of several research centers. Experts at Skoltech worked with biomaterials and immune cells, ITMO made a key contribution to the development of photosensitive nanomaterials and optical applications, while our colleagues from MIPT held biomedical studies,” says Mikhail Zyuzin, a chief researcher at ITMO and MIPT and one of the paper’s authors.

Top to bottom: 1) Carrier synthesis; 2) Scanning election microscope and confocal laser scanning microscope images of macrophages after carrier capture; 3) Diagram of switched macrophage share in mice tumors after carrier injection and laser treatment. Images courtesy of the researchers
The joint project by ITMO, MIPT, and Skoltech was launched with support from the federal program Priority 2030 (project Klever). The grant allowed scientists from different cities to collaborate on the new photothermal immunotherapy system. This project has been in development for two years.
At the moment, the macrophage switching method is at the stage of preclinical trials. Next, the researchers will proceed to animal studies to evaluate the effect of their method on tumor growth and regression. Additionally, the research team is considering opportunities to expand their collaborations with clinics for further development and implementation of the technology into clinical practice.