The conversation about needing to integrate new technologies into public health has been going on for a while, even since before the pandemic. But which technologies specifically are we talking about – and how can they help?
Public health technologies is a very wide-ranging concept. But first of all, it concerns the prevention of diseases and health issues that have a major impact on the public. There are three major groups:
- Cardiovascular diseases;
- Oncological diseases;
- A wide range of demographically significant issues related to the birth rate, quality of OB-GYN care, and childhood mortality rate.
The goal of public health technologies is to ensure timely diagnosis and prevention; to prevent the disease from worsening and begin treatment when full recovery is more likely. There are many ways to do that with the help of medical techniques and digital technologies – including AI. The latter is what we at ITMO are working on.
Of course, the pandemic has had an effect – but we always knew that with the population aging, pressure on the healthcare system would grow. In order to provide medical help to all who need it, we must adopt new ways of automating healthcare.
What would that look like?
I’ve already mentioned the need for early screening. Unfortunately, as we all know, diseases don’t always manifest themselves right away. If you consult a clinician too late, the health issue could be too severe to be treated properly.
That’s why we must identify issues early, including among asymptomatic patients. It’s not easy: such diagnostics require a lot of resources and increase the workload. After all, you’d need to test a great number of people and process thousands of samples. Secondly, where would you even find enough medical specialists to correctly examine such a massive amount of data from seemingly healthy people?
The solution to this issue lies with AI and automation, and more specifically – with autonomous analysis systems, such as the ones that interpret X-ray scans. Just a year ago, the first such system was registered in Europe. I should note that these systems don’t identify health issues, but merely use their databases to weed out samples that are free of pathologies and, therefore, allow clinicians to focus on the ones that could have cause for concern. This would allow us to run screening programs at a larger scale.

Anna Andreychenko. Photo by Dmitry Grigoryev / ITMO.NEWS
What is the state of such tech in Russia? I know that you’ve been a part of an experiment on the use of computer vision for medical purposes. What was the result?
I’ve worked on this project from 2019 to 2022. During the first stage, I was in charge of formulating the scientific approaches. The main goal was to conduct a study on the possible use of decision-making systems in the Moscow healthcare system, and more specifically in the analysis of X-ray scans. I would say that, at the moment, this is the only medical project in Russia where computer vision is applied in such a proactive and comprehensive fashion. This initiative is important on the global scale, too. Let me explain why.
The thing is, there is a central radiology service in Moscow that unites all radiology facilities run by the city’s Healthcare Department. Every day, this system receives results of more than 30,000 medical tests from all over town. By involving computer vision in this process, we were able to very quickly test the technology on a massive array of scans – pretty much on a citywide scale.
There aren’t many analogous services in the world. I know there’s something similar in China, but I’ve yet to hear anything about such projects in Europe or the US.
The project is still ongoing, but even the first stage has already shown that it’s possible to analyze this amount of data in real time and produce sufficiently reliable results. For the next stage, our goal is to demonstrate the clinical value of these algorithms. We've already laid the technological groundwork in order to establish a kind of “conveyor line” in terms of assessing, installing, testing, and maintaining AI algorithms.
In what ways will the project make the everyday work of clinicians easier?
First of all, the main advantage of automation is how quickly we can provide diagnoses. Secondly, it helps standardize and streamline the process.
X-ray scanning is rooted in a somewhat subjective approach. If you were to give the same image to two different clinicians, you will likely get different interpretations from both. That’s not an issue specific to Russia; all over the world, medical dictionaries, standardized databases, and report forms are developed in order to address this problem and achieve a uniform approach. Machines are helpful in this endeavor because they use specific data and compare the samples to a standard template. In order to develop such a template, we can’t rely on any one specialist – we must account for additional studies or seek a medical consensus. When we developed the datasets for our experiment, our task was to reach such a consensus on every study.
Read also:
How ITMO Trains Specialists in Public Health Sciences
Over 400 Clinicians From All Over Russia Attend (Non-)Conference at ITMO
Dr. Carlos Cabal From University of Havana on the Future of MRI
The medical community is known to be rather conservative. What did the clinicians think of the experiment? How can we increase public trust towards these technologies?
That’s a hard one. First, we need to work with mistrust towards these technologies through educating people about them – such automated systems shouldn’t be a black box for medical specialists. Moreover, we often have to deal with an irrational fear of technologies, as if they are some living organisms that have come to take over our jobs. This is not true: first and foremost, it is just a piece of software that works with a dataset, detecting various patterns. Once you realize it, you start seeing its limitations.
In order to promote the use of these solutions, we need public figures to demonstrate this through their own example, as well as legislation that would regulate this technology.
After all, the final decision remains with the clinician, which is why they are wary of using AI: if you are personally responsible for the result, you will naturally want to re-check whatever suggestion the system comes up with. This is why we need to regulate the share of responsibility.
For instance, in the case of an autonomous system, I would say that the manufacturer should bear part of the responsibility. The developers have to realize the consequences of any malfunctions in their products.
Credit: National Cancer Institute / Unsplash
What is the state of these issues in Russia?
The ethics of AI is still a nascent field in Russia, with Sberbank being one of its pioneers. 10 state standards for AI testing were developed in Moscow this year, including some for medical applications, but there are still many ethical questions surrounding AI both in Russian and international legislations.
You head a new lab at ITMO called Digital Public Health Technologies. What are the main objectives of your team?
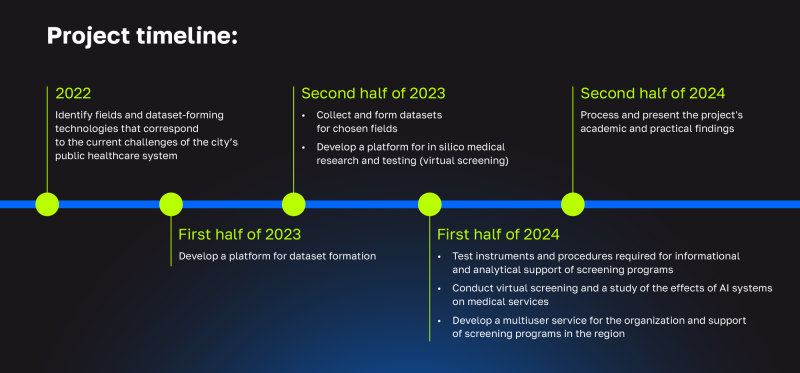
The lab was founded in November 2022 as part of the national project Science and Universities. Instead of aiming to develop new AI models, we see our main goal in creating technologies that will ensure safe and secure implementation of AI-based systems in practice.
Right now, we are working on a system of microservices that form medical datasets. For this, we need to solve various issues such as integrating our system with medical services and fine-tuning its interfaces for data collection and storage.
It’s only natural that hospitals and clinics do not have a data engineer on staff, so it’s our task as a leading IT university to provide technological solutions for them. Importantly, we don’t force any technologies on medical specialists – instead, we actively collaborate with them at the very early stages; they are the ones voicing their requests. This way, we can develop products that will be in demand in medical practice.
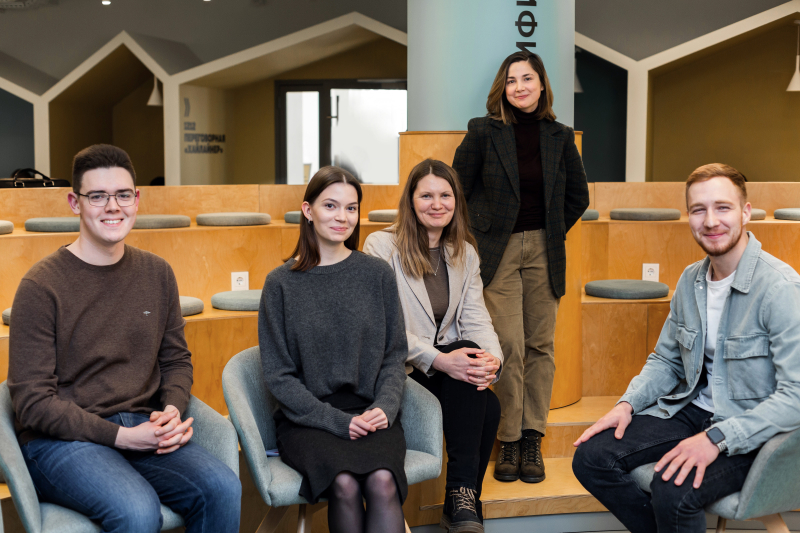
The lab’s team (left to right): healthcare economist Arsen Davitadze, science communicator and lab administrator Anna Uskova, medical physicist and head of the lab Anna Andreychenko, pulmonologist Nika Pushkina, and information security expert Stanislav Kondratenko. Photo by Maria Bakina / Megabyte Media
What are the products you are planning to develop?
The project that’s already underway is a support system for lung cancer screening. It’s part of a program launched by oncologist Andrey Nefedov from the National Research Institute of Pulmonology. Apart from developing the methodology, Dr. Nefedov found partners and coordinated the program. However, as the data was collected manually, there remained a high risk of error – for instance, if patients are assigned a wrong ID number, their data will not be processed correctly.
We suggested a system that would take over the job: it would ID a participant and attach their screening results, send any necessary files for review to responsible clinicians, structure the information, and forward at-a-glance analytics reports to the leading specialist for any additional decisions. At the moment, the system is designed specifically to accompany lung cancer screening, but it is module-based so that in the future we can adapt it for other purposes.
Following ITMO’s new policies, we are making an open-source product that will be available for anyone to use or adapt. We are hoping that as a result, we will demonstrate the project’s clinical efficiency and create a proven method of optimizing the screening process. The service will also be scalable – later, it might become a city-wide initiative.
Credit: dpht.itmo.ru
And what is the timeline of this work?
The MVP for this project is slated to be released this summer and in general the lab’s work is arranged around the national project, which spans 2022-2024. However, we are hoping that we will continue working afterward: the system currently in development can be used for other purposes, too, such as breast cancer screening.
Usually, during computer tomography (CT), medical specialists aim to identify a specific issue that matches the patient’s symptoms. However, the amount of data obtained during this kind of imaging can be used by an automated system to detect many other biomarkers that would’ve been impossible for a human to spot among the 300-500 images that make up the results of one regular lung computer tomography. Currently, all this data remains uninterpreted and unrecorded.
We will be collaborating with the N.N. Petrov National Medicine Research Center of Oncology to aggregate the CT images they have and test the existing AI systems for biomarker detection. This will allow us to evaluate the tools currently on the market and issue recommendations on the best one to be adopted in the city.

Anna Andreychenko. Photo by Dmitry Grigoryev / ITMO.NEWS
Apart from medical specialists, what interdisciplinary experts are part of your lab’s team?
Interdisciplinarity is crucial in medicine at every stage. A team working in public health sciences has to include clinicians, developers, and epidemiologists – the latter can outline the valid datasets needed for research on a specific illness, help with study design, and calculate the ultimate clinical value of AI systems. Also on our team are science communicators and sociologists, who help us establish collaboration with medical specialists and patients, raising their awareness of medical AI applications.
Is it possible to join your team?
We have many intern developers and we are very interested in involving students in our work and community, as well as giving them a base for their theses. We are also open for collaboration with medical organizations and clinicians who see the value of automatization and have a specific demand for such systems.






