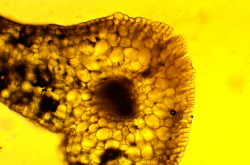
Immune thrombocytopenia (ITP) is a rare disease that causes the immune system to attack and destroy thrombocytes – the blood cells that help stop bleeding. A person with ITP may often have nosebleeds, their bruises may take longer to heal, and hemorrhages may occur in the skin and mucous membranes. Besides physical discomfort, the disease also affects daily life: patients face anxiety, restrictions on physical activity, and challenges with treatment.
ITP can develop at any age, but is most common in women and the elderly. Annually, from 3 to 6 people per 100,000 adults develop the condition; the disease is rarer in children. In Russia, the numbers are similar to those in other countries. For many adults, the disease becomes chronic and requires lengthy observation and therapy.
Even though it isn’t widespread, ITP has been studied quite well, with the existing treatments allowing patients to maintain their lifestyle. One such treatment is Nplate (also known as romiplostim or the synthetic protein AMG531), which is recommended by the Russian Ministry of Health and is on the list of essential medicines in Russia.
However, the original medicine is considered to be quite expensive, especially in countries with limited resources or in cases where patients require permanent therapy. That’s why pharmaceutical companies develop biosimilars: analogs of biological treatments that are just as effective and safe, but at the same time significantly cheaper.
It is to this effect that the Russian company GEROPHARM synthesized a new romiplostim biosimilar – protein GP40141. Recently, a group of researchers, including public health scientists from ITMO, have presented the results of the third and final trial of the treatment. 136 patients from 16 Russian medical centers took part in the study. They were sorted into two groups: one received the biosimilar GP40141, and the other – the original Nplate. The study aimed to evaluate the efficiency of the new treatment and whether it can help reach the necessary thrombocyte concentration in the blood.
After the tenth week of therapy, 78% of patients in the biosimilar group and 85% of patients receiving the original treatment showed a positive response (the necessary thrombocyte level). Moreover, the experiment demonstrated no significant differences in other efficiency indicators, including stability and duration of the treatment's effects. The biosimilar also proved to be safe: the frequency of side effects was identical to the original treatment, while all of them were light.
The researchers also note that the trials proved the low immunogenicity of the new treatment: only a few of the patients developed protein-cancelling antibodies – and even in these cases, they didn’t affect the therapy’s efficiency.
“Clinical trials are a complex and demanding process that requires a big team from both inside and outside the company conducting them. This study is interesting because it included patients who were already receiving Nplate therapy and transitioned to the biosimilar within the study. Thanks to this unusual methodology, we were able to not only acquire data on the effectiveness of the bioanalog, but also data on the safety of transition from the original treatments to its analog. This transition doesn’t lead to any changes in the safety and efficiency of the therapy,” says Ekateina Protsenko, a Master’s student of public health sciences at ITMO and a medical R&D advisor at GEROPHARM.
The research team was also able to introduce two important new aspects.
“First, we used in silico simulation to justify the endpoint and calculate the sample size; this allowed us to optimize the design of the study, making it shorter and less expensive. Second, it was the first time that we included patients that used to receive a different TPO antagonist, eltrombopag, and demonstrated that even with a weak response to previous therapy, a good response to a change of treatment is possible. This opens up new opportunities for therapy of such cases,” says Vladislav Kovalik, a graduate of the Public Health Sciences Master’s program.
The study aiming to evaluate the safety of prolonged treatment with the new medicine ended in January 2025. The new biosimilar has already been registered and will be available to patients as part of a national program. GEROPHARM will continue studying the medicine as part of an extensive safety evaluation in order to collect data on the long-term effects of the new romiplostim biosimilar.
“At GEROPHARM, we support the open-source research culture by publishing the results of our clinical trials. With this approach, we can ensure the transparency and accuracy of the data on the effectiveness and safety of our treatments. This is especially important for patients and the medical community,” says Roman Drai, the head of GEROPHARM’s research center.